Unrecognized effects undermine survivors’ ability to heal, Ohio-focused research finds
In 2017, Time magazine wrote about a study that found 110 of 111 deceased NFL players had a brain disorder caused by repeated head trauma.
The trauma was named as the main culprit in problems the football players had experienced with memory, bad moods, organizing simple and complicated ideas and tasks, as well as suicidal behavior.
The news was important but not surprising. Ohio, after all, had put a law on the books four years earlier outlining how concussions in young athletes should be treated because of their potentially serious effects.
Now Ohio advocates for domestic violence survivors are connecting the dots for a population whose most common injuries, according to the Centers for Disease Control and Prevention, involve the head, neck and face.
Rachel Ramirez, training director at the Ohio Domestic Violence Network, said the brain injury connection has been overlooked for far too long.
“What do we think when domestic violence survivors don’t show up for appointments, when we’re talking and we know they’re just not getting it?” she said. “What do we think when they’re not figuring out their lives? We might think they don’t care about their safety, they’re uncooperative, they’re lazy, you know?
“We have all of these different assumptions we make, and brain injury — which can cause every one of these behaviors — is not on the list at all.”
Funded by a federal grant obtained in 2016, ODVN has been researching the extent of the problem in Ohio and testing how best to alert abuse survivors — and the law enforcement, criminal justice and other professionals who work with them — to the implications of a blow to the head or strangulation.
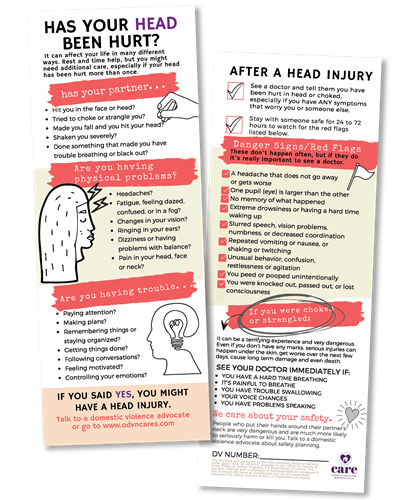
Advocacy tools developed in the study, including the one shown here, are available free for download at
www.odvn.org.
“We talked to survivors, and 81% had experienced hits to the head before accessing service,” said lead researcher Julianna Nemeth, an assistant professor at Ohio State University. “Fifty percent had experienced hits to the head so many times that they couldn’t even remember how many times. And strangulation, 83% of survivors had experienced it.”
Brain injuries don’t necessarily reveal themselves through bruises or cracked bones. The Mayo Clinic, a respected medical center in Rochester, Minnesota, says that even a mild injury to the brain “is still a serious injury that requires prompt attention and an accurate diagnosis.”
People who’ve dealt with such injuries have experienced short- and long-term impairment to memory and reasoning, sensitivity to light and noise, tremors and seizures, nightmares and flashbacks, and difficulty controlling emotions.
For domestic violence survivors, such problems might result in an inability to recall what happened to them, to find their way to the courthouse or remember an appointment, or to plan what they would need to do to escape a dangerous situation.
“Those are all very complicated brain functions,” Ramirez said. “We take it for granted. But for survivors, you have this person who is not able to do something they used to be able to do and who has no idea why. These people think they’re going crazy — and, of course, they do because they’ve been told by their abusers that they are crazy.”
One survivor Ramirez knows, a woman named Paula who worked as an emergency medical technician in the Toledo area, experienced exactly that.
Amid ongoing abuse, her partner almost strangled her to death. She suffered brain injuries that she didn’t know about and, as a result, nightmares, flashbacks and a sensitivity to noise that would trigger an overreaction for which she then hated herself. She self-medicated with alcohol.
“Paula went to a therapist and said: ‘I think I’m crazy. Put me in a psychiatric ward,’” Ramirez said.
Paula’s brain injuries went undiscovered until she was in a car accident and underwent an MRI.
Such accidental discovery is common, Ramirez said. In fact, in Nemeth’s research, survivors said service providers rarely talked about brain injury and service providers — those who work with survivors every day — reported having met very few with brain injuries.
They did, however, report a disproportionate number of survivors who experienced seizures.
“Not all survivors of domestic violence have brain injuries,” Nemeth said, “but our message to agencies has really become, ‘You basically have to assume that a survivor coming to your services has an unmet need regarding a potential brain injury.’
“We’ve really stumbled upon this huge unmet need,” she said.
Most of the research on people who’ve suffered brain injuries has involved privileged subsets of the population, such as NFL players.
“We were at a brain injury conference last week,” Ramirez said, “and there was a presenter who studied 10 private schools in Connecticut with an average tuition of $50,000. The focus was educating athletic trainers.”
Which isn’t to say that athletes’ concussion-related injuries aren’t important, Ramirez and Nemeth said.
“It’s just that the frameworks that have been built for intervention regarding brain injury, they don’t apply to this population of survivors,” Nemeth said.
Doctors tell those who’ve suffered brain injuries to rest and avoid stress.
“That’s exactly how you do it when you have a kid who is in soccer and has a concussion,” Ramirez said. “But what does that look like in the domestic violence world?”
The Ohio Domestic Violence Network didn’t explore the clinical science, but it aimed to do two things: develop a care framework that recognizes victims’ vulnerability to brain injuries and help advocates adjust programs to give survivors a better chance for success and thus healing.
For the research, Nemeth and her team worked with five agencies in Ohio focused on domestic violence survivors. Staff members, administrators, volunteers and survivors were interviewed.
Next came development of the care framework (named CARE, for
connect,
acknowledge,
respond,
evaluate) and support tools, which in part help survivors recognize how a brain injury might affect them. The researchers designed an evaluation process to look at whether survivors exposed to the care framework experienced better results.
With the work now in the end stages, the team is writing final reports and planning for a statewide rollout, Ramirez and Nemeth said.
The benefits of the study, Nemeth said, extend beyond domestic violence shelters.
“This doesn’t just have applications for how it is that we bring survivors into shelter services,” she said. “It has applications for how we’re interacting with survivors in every system that they come in contact with.
“In terms of criminal justice, law enforcement, we have agencies that are using this ‘Has your head been hurt’ card when they go out to the scene of domestic violence calls. We have hospital emergency rooms that have called to say: ‘Thank you so much for sending this card. We never would have thought about assessing for brain injury, but, because of the card, we did — and that’s exactly what we needed to do.’”
For more details, contact Ramirez at rachelr@odvn.org. Funding for the study was provided by the U.S. Office for Victims of Crime under grant 2016-VX-GX-K012.